This page is intended for Healthcare Professionals.
Professional resources
RESOURCES FOR CLINICIANS AND YOUR PATIENTS
Download, print, or email useful clinician and patient resources about Rebif® and treating relapsing multiple sclerosis (RMS)
RESOURCES FOR CLINICIANS AND YOUR PATIENTS
Download, print, or email useful clinician and patient resources about Rebif® and treating relapsing multiple sclerosis (RMS)
Resources for clinicians
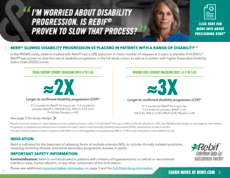
EDSS: Expanded Disability Status Scale.
†PML: progressive multifocal leukoencephalopathy
Resources for patients
INDICATION AND IMPORTANT SAFETY INFORMATION
for REBIF® (interferon beta-1a) for subcutaneous injection
INDICATION
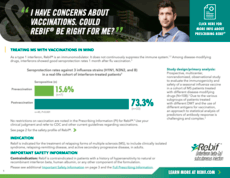
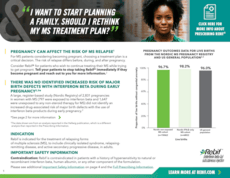
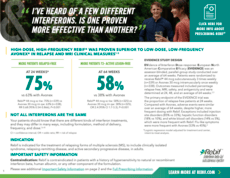
Rebif is indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
IMPORTANT SAFETY INFORMATION
Contraindication: Rebif is contraindicated in patients with a history of hypersensitivity to natural or recombinant interferon beta, human albumin, or any other component of the formulation.
Depression and Suicide: Use Rebif with caution in patients with depression, a common condition in people with multiple sclerosis. Depression, suicidal ideation, and suicide attempts have been reported to occur with increased frequency in patients receiving interferon compounds, including Rebif.
Hepatic Injury: There have been rare reports of severe liver injury, including some cases of hepatic failure requiring liver transplantation, in patients taking Rebif. Consider the potential for hepatic injury when Rebif is used in combination with other products associated with hepatotoxicity. Monitor liver function tests and patients for signs and symptoms of hepatic injury. Consider discontinuing Rebif if hepatic injury occurs.
Anaphylaxis and Other Allergic Reactions: Anaphylaxis and other allergic reactions (some severe) have been reported. Discontinue Rebif if anaphylaxis occurs.
Injection Site Reactions Including Necrosis: In controlled clinical trials, injection site reactions occurred more frequently in Rebif-treated patients than in placebo-treated and Avonex-treated patients. Injection site reactions including injection site pain, erythema, edema, cellulitis, abscess, and necrosis have been reported in the postmarketing setting with the use of Rebif. Do not administer Rebif into affected area until fully healed; if multiple lesions occur, change injection site or discontinue Rebif until skin lesions are healed. Some cases of injection site necrosis required treatment with intravenous antibiotics and surgical intervention (debridement and skin grafting). Some cases of injection site abscesses and cellulitis required treatment with hospitalization for surgical drainage and intravenous antibiotics. Rotate site of injection with each dose to minimize likelihood of severe injection site reactions, including necrosis or localized infection.
Decreased Peripheral Blood Counts: Decreased peripheral blood counts in all cell lines, including pancytopenia, have been reported in Rebif-treated patients. In controlled clinical trials, leukopenia occurred at a higher frequency in Rebif-treated patients than in placebo and Avonex-treated patients. Thrombocytopenia and anemia occurred more frequently in 44 mcg Rebif-treated patients than in placebo-treated patients. Monitor patients for symptoms or signs of decreased blood counts. Monitoring of complete blood and differential white blood cell counts is also recommended.
Thrombotic Microangiopathy: Cases of thrombotic microangiopathy (TMA), some fatal, have been reported with interferon beta products, including Rebif, up to several weeks or years after starting therapy. Discontinue Rebif if clinical symptoms and laboratory findings consistent with TMA occur and manage as clinically indicated.
Pulmonary Arterial Hypertension: Cases of pulmonary arterial hypertension (PAH) have been reported in patients treated with interferon beta products, including REBIF. Patients who develop unexplained symptoms (e.g., dyspnea, new or increasing fatigue) should be assessed for PAH. If alternative etiologies have been ruled out and a diagnosis of PAH is confirmed, discontinue treatment and manage as clinically indicated.
Seizures: Seizures have been temporally associated with the use of beta interferons, including Rebif, in clinical trials and in postmarketing reports. Monitor for seizures when administering Rebif to patients, particularly those with pre-existing seizure disorders.
Laboratory Tests: New or worsening thyroid abnormalities have developed in some patients treated with Rebif. Thyroid function tests are recommended every 6 months in patients with history of thyroid dysfunction or as clinically indicated.
Adverse Reactions: The most common side effects with Rebif are injection-site disorders, influenza-like symptoms, abdominal pain, depression, elevated liver enzymes, and hematologic abnormalities.
Pregnancy: Epidemiological data do not suggest a clear relationship between interferon beta use and major congenital malformations, but interferon beta may cause fetal harm based on animal studies. Data from a large human population-based cohort study, as well as other published studies over several decades, have not identified an increased risk of major birth defects with exposure to interferon beta products during early pregnancy. Findings regarding a potential risk for low birth weight or miscarriage with the use of interferon beta products in pregnancy have been inconsistent.
Lactation: Limited published literature has described the presence of interferon beta-1a products in human milk at low levels. There are no data on the effects of interferon beta-1a on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for REBIF and any potential adverse effects on the breastfed child from REBIF or from the underlying maternal condition.
To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono, Inc. at 1-800-283-8088 ext. 5563 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Please see Full Prescribing Information and Medication Guide.
References: 1. PRISMS Study Group. Randomised double-blind placebo-controlled study of interferon β-1a in relapsing/remitting multiple sclerosis. Lancet. 1998;352(9139):1498-1504. 2. Data on file. EMD Serono, Inc. PRISMS study report. 3. Data on file. EMD Serono, Inc. PRISMS 2010 Confirming analysis. 4. Rebif® [Prescribing Information]. Rockland, MA: EMD Serono, Inc. 5. Freedman MS, Brod S, Wray S, et al. Post hoc Analysis to Evaluate the Effects of Subcutaneous Interferon beta-1a in Subgroups of Patients from the PRISMS Study with Early Onset Versus Late Onset Disease. Poster presented at: ECTRIMS 2019; 11-13 September; Stockholm, Sweden. 6. Li DKB, Paty DW; UBC MS/MRI Analysis Research Group, PRISMS Study Group. Magnetic resonance imaging results of the PRISMS trial: a randomized double-blind, placebo-controlled study of interferon-β1a in relapsing-remitting multiple sclerosis. Ann Neurol. 1999;46(2):197-206.